

cap-ONE

What is cap-ONE?
cap-ONE is Nihon Kohden's unique mainstream CO2 sensor for both intubated and non-intubated patients. The ultra compact sensor and unique adapter provide accurate measurements and reduce the burden on the patient.
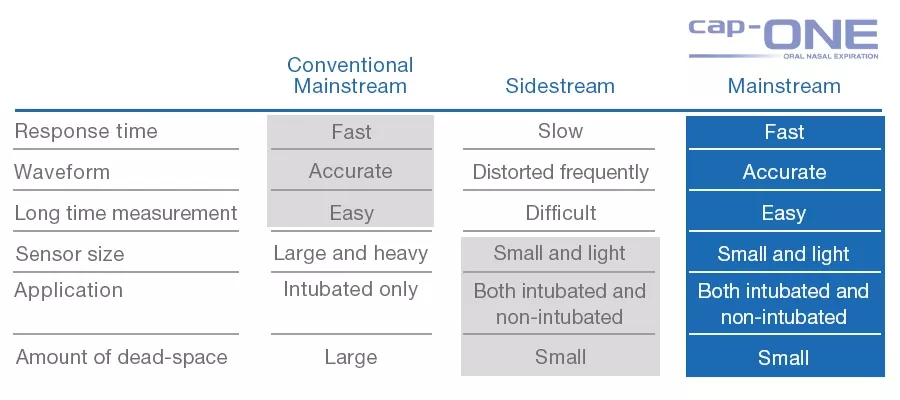
cap-ONE overcomes the disadvantages and maintains all the advantages of mainstream sensor for the optimal capnography.
Feature
Heaterless and motorless structure
Our CO2 sensor is ultra-compact weighing only 4 g, with a heaterless and motorless structure, that meets the United States Military Standard* for shock resistance.
*United States Military Standard: a performance test standard for products used by the US military. This is one of the evaluation standards for products in harsh environments.
Our two mainstream CO2 sensors
Based on the principle of infrared absorption spectroscopy, Nihon Kohden provides two mainstream CO2 sensors: Quantitative method and Semi-quantitative method.
Why is CO2 monitoring important?
CO2 measurement can predict hyperventilation or hypoventilation which can be caused by inadequate analgesia, sedation or other potentially life-threatening causes.
Recommendations from guidelines and studies
Ensures quality of CPR and is an early indicator for ROSC1
- A value of less than 10 mmHg is associated with failure to achieve ROSC and may indicate that the quality of chest compressions should be improved.
Detect ventilator troubles
- 8-25% of anesthesia accidents were reported as being due to breathing circuit problems.
- Breakdown of breathing circuit problems: Circuit disconnection 8-15%, Misconnection of circuits 2-4%, Displacement of endotracheal tube 2-6%.
Avoid unrecognized esophageal intubation2
- Patients worldwide die every year from unrecognized esophageal intubation, which is an avoidable complication of airway management usually resulting from human error.
- Checking correct tracheal tube placement using capnography for identification and monitoring of expired carbon dioxide (CO2) is necessary to avoid human error.
Reduce frequency of hypoxemic events3, 4
- Continual monitoring of ventilatory function with capnography to supplement standard monitoring by observation and pulse oximetry is recommended to address moderate procedural sedation and analgesia.
- Access to capnography provides fewer but more timely interventions for hypoventilation, which leads to fewer episodes of hypoventilation and of oxygen desaturation.
Assists in better patient care and outcomes5
- The monitoring of ventilation using capnography is vital for titrating sedatives to which different patients have variable levels of sensitivity, and provides early warning signs of adverse respiratory events.
1 Part 3: Adult Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care | Circulation (ahajournals.org)
2 Paul A. Baker Unrecognisedoesophagealintubation: time for action –ScienceDirect
3 Practice Guidelines for Moderate Procedural Sedation and Analgesia 2018 | Anesthesiology | American Society of Anesthesiologists (asahq.org)
4 Langhan, M. L., Shabanova, V., Li, F. Y., Bernstein, S. L., & Shapiro, E. D. (2015). A randomized controlled trial of capnography during sedation in a pediatric emergency setting.The American journal of emergency medicine,33(1), 25–30.
5 Use of Capnography during Moderate Sedation by Non-Anesthesia Personnel in Various Clinical Settings -Anesthesia Patient Safety Foundation (apsf.org)
Our two mainstream sensors
Quantitative method
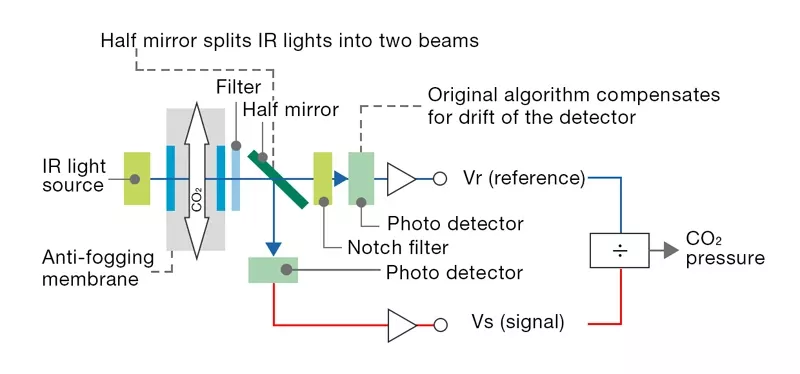
In quantitative method, the infrared light transmitted through the airway adapter is split into two by a half mirror. One of which is detected as a signal output (Vs), The other passes through the gas cell* and detected by another photo detector as the standard output (Vr). The partial pressure is calculated from the ratio of this signal output Vs and standard output Vr.
*gas cell: a cell containing 100% CO2 gas
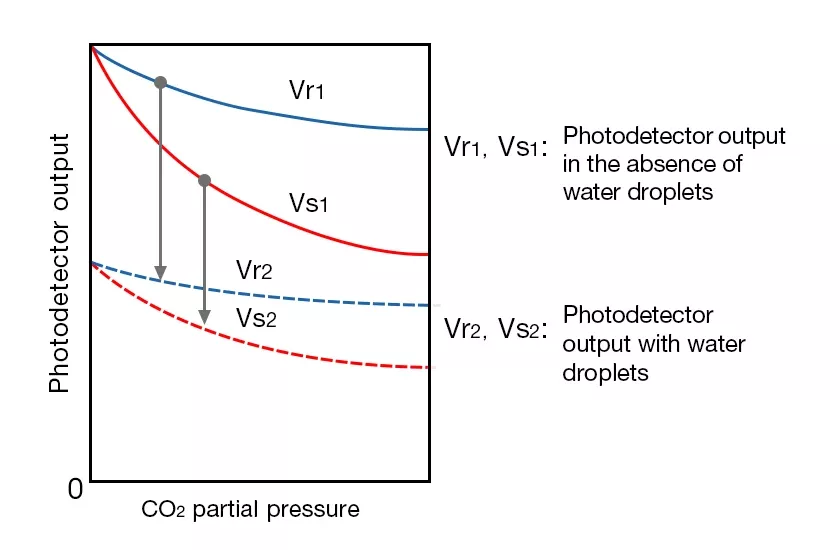
This measurement method is suitable for measurement when nebulizers are used or when humidification is used.
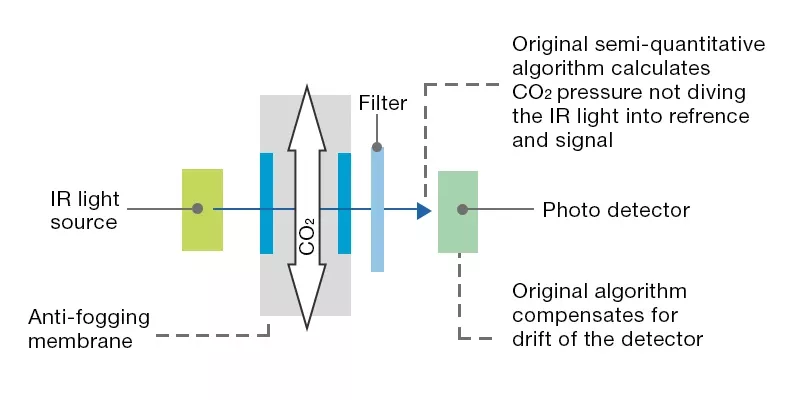
Semi-quantitative method
Simple structure consisting only of an infrared light source, filter, and photodetector.
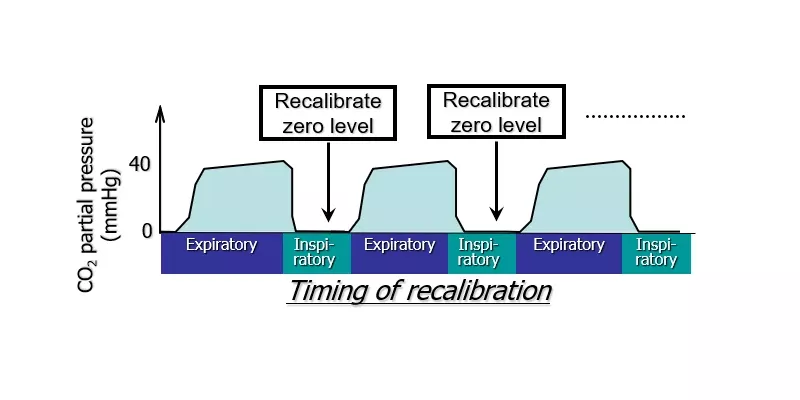
CO2 is barely found in inspiration. This means that the CO2 level of the inspiration can be assumed as 0 mmHG and zero calibration can be automatically performed for each inspiration. CO2 partial pressure is calculated from the amount of infrared transmission (output of the photo detector) of exhalation and inhalation.
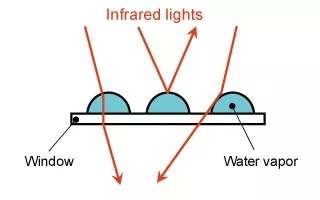
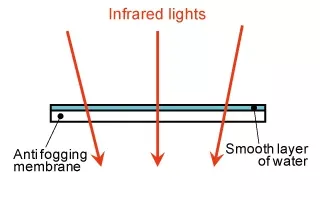
Innovative features—Anti-fogging membrane
cap-ONE uses an original transparent film with an anti-fogging membrane. It forms a smooth layer of water which allows stable transmission of infrared light without irregular reflection. This technology eliminates the need for heaters and reduces the power consumption and weight of the sensor.
Without anti-fogging membrane | With anti-fogging membrane inside the airway |
Image
| Image
|
Image
| Image

|
Improving manual ventilation and CPR with ETCO2 Audible Cue

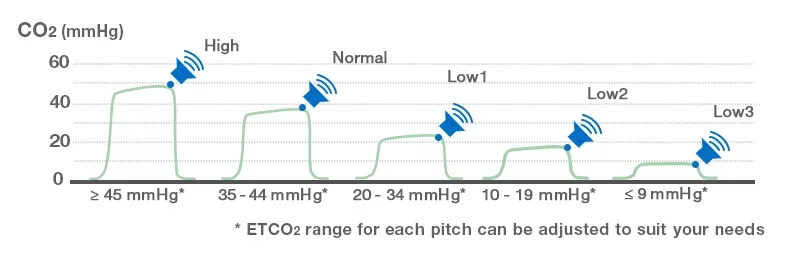
The actual Audible Cue sounds
| Primarily designed for | ETCO2 Range | Sound Type | Sound Design | Example of Situation | Sound |
| Manual ventilation and ROSC confirmation | High 45≤ | Image

| Image

|
| |
| Normal 35-44 | Image
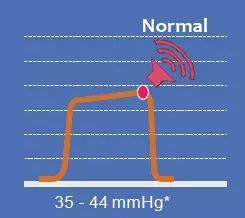
| Image
| Ventilation is sufficient | ||
| Low1 20-34 | Image

| Image

| Hyperventilation is caused by over aggressive manual ventilation during transport | ||
| CPR (Chest compression) | Low2 10-19 | Image
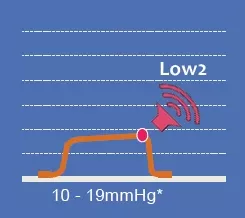
| Image
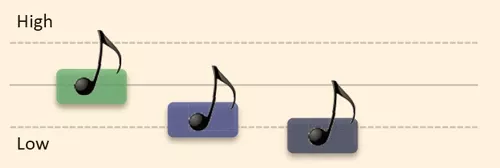
| High quality chest compressions are achieved | |
| Low3 ≤9 | Image
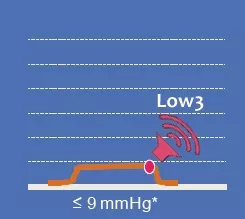
| Image
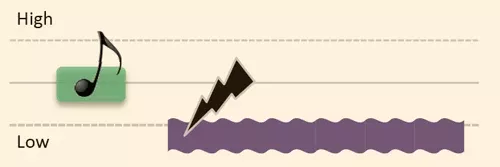
| Quality of effectiveness of chest compression may need improvement |
ROSC: Return of Spontaneous Circulation
자료 다운로드—cap-ONE
Learn more

Monitor Your Patient with Reliable cap-ONE Mainstream CO2 Sensor

Ensure Quality of Care under Sedation

Optimal respiratory monitoring during sedation for all patients

Improve Manual Ventilation and CPR with ETCO2 Audible Cue





